Trigeminal Neuralgia
Trigeminal neuralgia is a chronic pain condition that involves the 5th cranial or trigeminal nerve (the fifth cranial nerve, also called the fifth nerve, or simply CNV or CN5). The trigeminal nerve is responsible for sensation in the face. Sensory information from the face and body is processed by parallel pathways in the central nervous system. The fifth nerve is primarily a sensory nerve, but it also has certain motor functions (biting, chewing, and swallowing).
Distribution of the Trigeminal Nerve
Trigeminal neuralgia is frequently described as one of the most painful experiences known to man. In the earlier days of my practice there were few effective ways of treating this disorder and trigeminal neuralgia earned the nickname "the suicide disease," due to the unfortunate and drastic steps some patients would take when they despaired of ever finding any relief. Trigeminal neuralgia is a pain that the patient describes as being sharp, stabbing, burning, boring or electrical pain that involves one side of the face. Patients are considered to have Type 1 trigeminal neuralgia if more than 50 percent of the pain they experience is sudden, intermittent, sharp and stabbing, or shock-like. These patients may also have some burning sensation. Type 2 trigeminal neuralgia involves pain that is constant, aching, or burning more than 50 percent of the time. Trigeminal neuralgia is typified by attacks that stop for a period of time and then come back. The attacks often worsen over time, with fewer and shorter pain-free periods before they recur. Trigeminal neuralgia can be debilitating due to the intensity of the pain, and some patients may avoid daily activities because they fear an impending attack.
Image #1: Distribution of the Trigeminal Nerve
Image #2: The generation of trigeminal nerve pain is thought to result from peripheral pathology (i.e. neurovascular compression) and central pathophysiology (i.e. hyperactivity of the trigeminal nerve nucleus).
Image #2
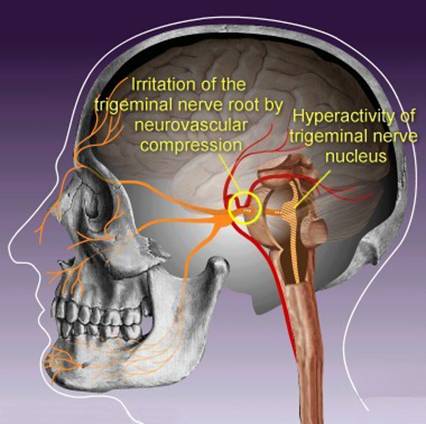
Trigeminal neuralgia typically presents in the dental malpractice forum when there is some type of trauma to a branch of the trigeminal nerve. Trigeminal neuopathy or post-traumatic trigeminal neuralgia may develop. This can result from extraction, implant placed into the inferior alveolar nerve, injury to the inferior alveolar nerve during a root canal procedure, excessive trauma to the jaw joint by an overly lengthy procedure, sinus injury from Caldwell-Luc procedures and following nerve destruction procedures (rhizotomies). Following an injury to the trigeminal nerve, initial numbness and paresthesia may become associated with bothersome sensations or pain, sometimes called phantom pain or deafferentation pain. These pain conditions are caused by irreparable damage to the trigeminal nerve and secondary hyperactivity of the trigeminal nerve nucleus.
In short, injury to the any of the branches of the trigeminal nerve can set in motion a trigeminal neuralgia that must be timely treated. The strongest evidence that a trigeminal neuralgia was caused by dental negligence is the chronological relationship to the subject dental trauma and the extent of the trauma. The defense will always argue that the two events are a mere coincidence. Depending on the nature of the original negligent act, the jury will be less likely to buy the defense argument.
Trigeminal neuralgia is usually brought on or exacerbated by "trigger points" such as touching the face, eating or chewing. Trigeminal neuralgia is frequently misdiagnosed as a dental condition in its early stages that results in unneeded extractions and root canals that do not resolve the condition. Radiographic studies (MRI, CBCT and CT scans) all appear normal and the condition is usually diagnosed by the patient's medical history and description of their pain complaints.
Treatment options for trigeminal neuralgia include medicine, surgery, and botox injections. Some patients will augment the above with acupuncture, biofeedback, vitamin therapy, nutritional therapy, and electrical stimulation of the nerves, with less certain results. Medications are the first line of treatment for trigeminal neuralgia and include carbamazepine (Tegretol®), phenytoin (Dilantin®), gabapentin (Neurontin®) and baclophen (Lioresal®). These anticonvulsant medicines are generally effective in treating trigeminal neuralgia and are prescribed to block nerve firing. Tricyclic antidepressants such as amitriptyline (Elavil®, Endep®, Vanatrip®) or nortriptyline (Aventyl HCl®, Pamelor®) are used to treat pain that is described as constant, burning, or aching. Typical analgesics and opioids are not usually helpful in treating the sharp, recurring pain caused by trigeminal neuralgia. Your best course of action is to seek treatment by an orofacial pain specialist who will seek to bring your pain symptoms under control by trying a varied regimen of these medications. It has been my experience in the last 10 years that most patients are effectively treated with a combination of these medications which are customized to each patient. If medication fails, some patients receive excellent results with botox injections into their trigger points where the trigeminal nerve becomes over stimulated. This treatment should be undertaken by a specialist and unfortunately is very expensive and lasts only 3 months for each series of injections. Often this therapeutic approach can result in a gradual diminishing of the trigeminal neuralgia symptoms over time. When medication and botox injections fail to relieve pain or produces intolerable side effects such as excess fatigue, surgical treatment may be recommended.
There are several neurosurgical procedures available to treat trigeminal neuralgia. The procedure that is recommended will depend on a variety of factors including your health and the trigeminal distribution that is involved. Some of these surgeries are done as outpatient procedures and some are done under general anesthesia in an inpatient setting. A rhizotomy is a procedure in which select nerve fibers are destroyed to block pain. A rhizotomy for trigeminal neuralgia causes some degree of permanent sensory loss and facial numbness, so most patients look to these procedures only after medication and/or botox injections have failed . Several forms of rhizotomy are available to treat trigeminal neuralgia, including balloon compression surgery, glycerol injection,radiofrequency thermal lesioning, stereotactic radiosurgery (gamma-knife surgery).
Microvascular decompression is performed under general anesthesia and is the most invasive of these surgical procedures, but it does not result in permanent nerve damage. The aim of microvascular decompression surgery is to alleviate neurovascular compression upon the trigeminal nerve root and therefore is a surgery which is used to treat trigeminal neuralgia which was not caused by dental trauma. Neurectomies (surgical severing of the trigeminal nerve) always results in numbness to the area this nerve serves and may not be a permanent remedy.
The best book on this subject for the patient is "Striking Back (Striking Back The Trigeminal Neuralgia and Face Pain Handbook 2004)".
For further discussion see the following organizations:
The National Institute of Neurological Disorders and Stroke

