Periodontics and Malpractice
The failure of the dental professional to diagnose and timely treat periodontitis is dental malpractice. The permanent damage a patient sustains from periodontitis usually occurs over a long period of time. In a dental malpractice case involving the failure to timely diagnose and treat the periodontitis, multiple dentists may be involved. The dental malpractice attorney will need all of your dental records for a period of 10 years, so an evaluation can be made as to when the disease process should have first become evident to the treating dentist/dental hygienist and which dental office is responsible and to what extent for the total damage sustained by the patient. The Failure To Diagnose Periodontitis is a silent killer of teeth. The patient will normally be unaware that the disease process is slowly removing the supporting structures of the tooth, until it is too late. It is the patient's obligation to see the dentist at least once and preferably twice a year. It is the dentist's obligation to perform regular oral examinations, take a full mouth set of x-rays every 2 years and perform regular periodontal probings, so that periodontitis can be diagnosed early and permanent damage to the patient's gums, bone and other supporting tooth structures can be avoided. The American Academy of Periodontology states that the following comprehensive steps must be taken by the dentist to comply with the standards of care in treating patients
1. Medical History
A medical history should be taken and charted by the dentist to evaluate and identify identify conditions that may predispose a patient to periodontitis or may affect treatment, patient management and/or outcomes. Such conditions include diabetes, hypertension, pregnancy, smoking, substance abuse and medications. When there is a condition that in the judgment of the dentist requires further evaluation, consultation with the patient's physician should be obtained.
2. Dental History
A dental history, including the chief complaint or reason for the visit, should be taken, charted and evaluated. Information about past dental and periodontal care and records, including radiographs of previous treatment, may be useful.
3. Extraoral Examination
Extraoral structures (outside the mouth) should be examined and evaluated. The temporomandibular apparatus and associated structures may also be evaluated.
4. Intraoral Examination Of The Patient's Soft Tissues
Intraoral tissues and structures, including the oral mucosa, muscles of mastication, lips, floor of mouth, tongue, salivary glands, palate, and the oropharynx, should be examined and evaluated.
5. Intraoral Examination Of The Patient's Teeth, Fillings, Crowns, Bridges and Implants
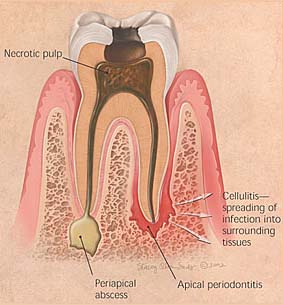
The teeth and their replacements should be examined and evaluated. The examination should include observation of missing teeth, condition of restorations (fillings, crowns and bridges), tooth decay, tooth mobility, tooth position, how the teeth come together when chewing, signs of abnormal wear from the patient grinding or clenching their teeth and signs of existing pulpal infections that may require root canals (See Image 1 and 2).
Image #1: Complete Exam Can Reveal Multiple Periodontal Problems
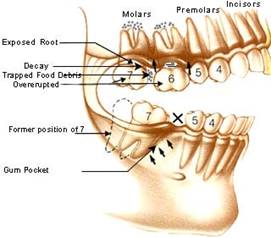
Image #2: Periapical Abscess and Apical Periodontitis
6. Radiographs
A base line set of radiographs that are current, including a full mouth set of periapical radiographs (FMX) should be taken for proper evaluation of the patient periodontium and dental implants (See Image 3). Radiographs of diagnostic quality are necessary for these purposes and radiographic abnormalities should be noted in the dental chart (See Images 4 and 5).
Image #3: Full Mouth Set Of Radiographs
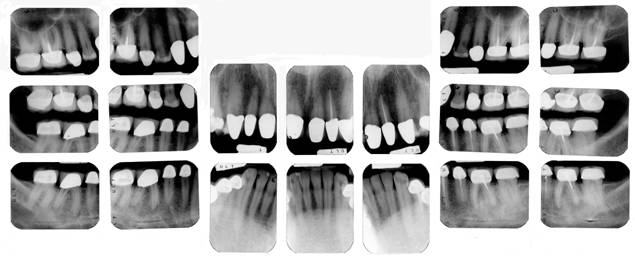
Image #4: Periapical X-Ray Showing Alveolar Bone Loss
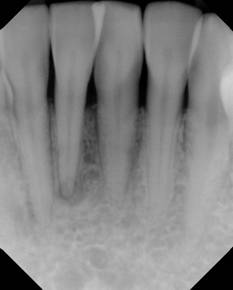
Image #5: Bitewing X-Ray Showing Alveolar Bone Loss

7. The Status Of Plaque And Calculus
The presence and distribution of plaque and calculus should be determined by probing (See Image 6) and x-rays (See Image 7). Plaque is a sticky, colorless deposit of bacteria that is constantly forming on the tooth surface. Saliva, food, and fluids combine to produce these deposits that collect on teeth and where teeth and gums meet. The buildup of plaque is the primary factor in periodontal (gum) disease. Fighting plaque is a life-long part of good oral care. Plaque begins forming on teeth 4 to 12 hours after brushing, which is why it is so important to brush at least twice a day and floss daily. Tartar, also called calculus, is a crusty deposit that can trap stains on the teeth and cause discoloration. It creates a strong bond that can only be removed by a dental professional. Tartar formation may also make it more difficult to remove new plaque and bacteria.
Image #6
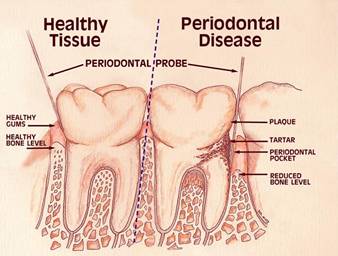
Image #7

8. Periodontal Examination
Periodontal soft tissues, including peri-implant tissues, should be examined. Do the gums look inflamed, red, is there pus present, do the gums look recessed around the teeth ("long in the tooth"), does the gum tissue have its normal stippling, are there other tissue abnormalities. In other words, do the gums and soft tissues appear healthy to visual examination (See Image 8)?
Image #8: Visual Exam With Probing Depths
9. Probing Depths
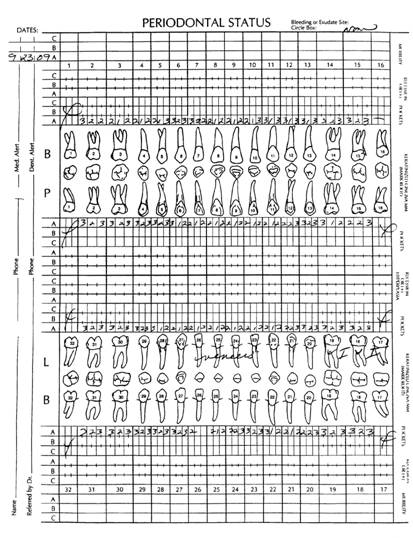
Probing depths, location of the gingival margin (clinical attachment levels), and the presence of bleeding on probing should be evaluated and charted systematically. Periodontal probing is essential as an original baseline to assess whether the treatment plan is working. The dentist is required to use a periodontal probe (See Image 9) and slide it along the tooth and below the gumline into the gingival sulcus to measure the probing depths around the entire tooth at 6 different locations (See Image 1, 10 and 11) and maintain a periodontal probing chart if disease is identified (Image 12).
Image #9:Periodontal Probe

Image #10
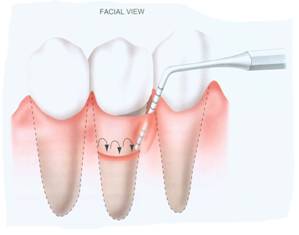
Image #11
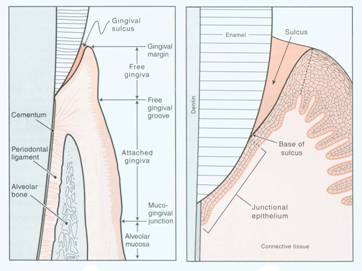
Image 12
10. Furcation Involvement
The presence, location, and extent of furcation invasions should be determined and charted. The furcation is the intersection of multiple roots under the crown (See Figure 13, 14 and 15).
Image #13: The Furcation

Image #14: Probing The Furcation

Image #15: X-Ray of Furcation

11. Additional Testing
In addition to conventional methods of evaluation; i.e., visual inspection, probing, and radiographic examinations, the patient’s periodontal condition may warrant the use of additional diagnostic aids. These include, but are not limited to, diagnostic casts, microbial and other biologic assessments, radiographic imaging, or other appropriate medical laboratory tests.
12. Charting
All relevant clinical findings should be documented in the patient’s record (See Perio Charting.wmv and Figure 17).
13. Referral To Periodontist
It is within the standard of care for a general dentist to monitor and treat a periodontal condition, however, if a general dentist elects to treat a patient's periodontal condition, that dentist is held to the standard of care that a trained periodontist would give the patient. Referral to a periodontist or other health care provider should be made and documented when warranted. A patient's refusal to follow a dentist's recommended referral to a periodontist should also be charted.
14. Treatment Plan
Based on the results of the dentist's examination, a diagnosis and proposed treatment plan should be presented to the patient. Patients should be informed of the disease process, therapeutic alternatives, potential complications, the expected results and their responsibilities in treatment. Consequences of no treatment should be explained to the patient.

