Periodontics Defined
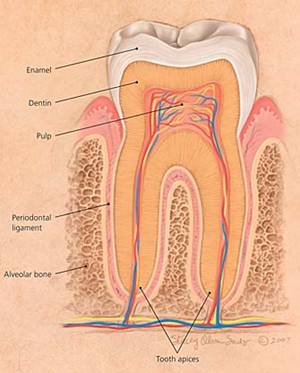
The word periodontics comes from the combination of the Greek roots, peri (around or about) and odons (tooth). Periodontitis is a bacterial gum infection that can lead to the destruction of the gums, bone and fibers that support your teeth (the periodontium). The periodontium is made up of gums (gingivae), periodontal ligament and alveolar/supporting bone (see Figures O and 1). Periodontitis can usually be easily treated when discovered early. Signs of periodontitis may include tenderness, bleeding gums, swelling of the gums or loose teeth, but the patient may have no signs whatsoever. If you have been seeing a dentist regularly over the course of many years, it is almost always dental malpractice if your dentist has failed to diagnose the condition before you have sustained permanent damage and bone loss.
Periodontium
Gingivitis and Periodontitis
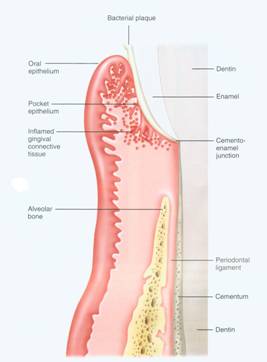
Gingivitis and periodontitis are the 2 major forms of inflammatory diseases affecting the periodontium. Their primary cause is bacterial plaque, which releases toxins that cause the living supporting structures for the tooth (gums, periodontal ligament and alveolar bone) to withdraw from the toxins and thereby leading to the destruction of this support if the bacterial plaque is not removed (see Image 2 and 3).
Image #2

Image #3

Gingivitis is inflammation of the gingiva that does not result in loss of this periodontal support. Periodontitis is inflammation of the gingiva and the adjacent periodontium and is characterized by the loss of gums, periodontal ligament and alveloar bone. Gingivitis is a reversible disease. Therapy is aimed primarily at plaque control and reduction or elimination gum (gingival) inflammation, thereby allowing gum tissues to heal, followed by appropriate patient hygiene instruction, dentist monitoring and teeth cleanings to prevent re-initiation of inflammation. (See Images 4 and 5); (See also, The American Academy of Periodontology at https://www.perio.org/for-patients/gum-disease-information/).
Image #4

Image #5
Therapeutic approaches for periodontitis fall into 2 major categories: 1) Stop the Problem: eliminate infection, deep cleanings, identification of those factors that are leading to the loss of periodontal attachment and removal or control of these factors; and 2) Surgery and Therapy: restore the structures around the tooth which were destroyed by disease. Essential to both treatment approaches is the use of timely recall visits to the dentist which are consistent with the severity of the periodontal problem.
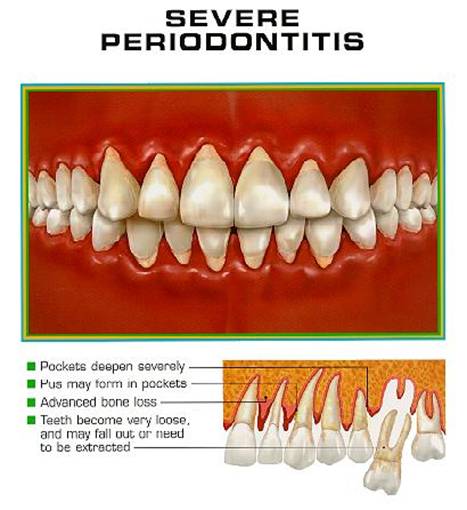
The stages of perodontitis are early periodontis (see Figures 6), moderate periodontitis (see Image 7-8) and severe periodontitis (see Image 9).
Image #6

Image #7

Image #8
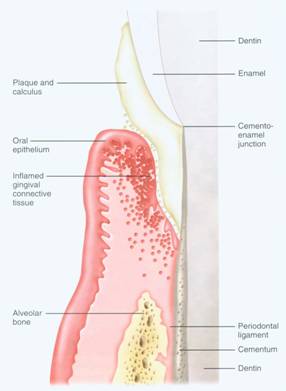
Image #9
The failure of a dentist to diagnose and treat periodontal disease can lead to the loss of teeth and can have serious medical consequences for the patient. Untreated chronic periodontal disease has been shown to contribute to poor systemic health. As in other infections, when you have periodontitis, your body tries to fight it to stay healthy. Scientists believe that this fight produces byproducts and chemicals that can travel through your blood stream into other parts of your body. Periodontal disease has been linked to:
- Cardiovascular disease (blood vessels of the heart)
- Peripheral vascular disease (blood vessels of the body)
- Endocarditis (inflammation of the inside lining of the heart chambers and heart valves)
- Strokes
- Poor control of blood sugar among diabetics
- Pre-term labor, intra-uterine growth restriction (IUGR), and low birth-weight babies
It is the obligation of the dentist to diagnose this condition and educate the patient with respect to proper oral hygiene and an appropriate recall schedule to actively manage and prevent its progression. If the periodontitis is too advanced to respond to conservative treatment, the dentist is obligated to refer the patient to a periodontist.

