Cone Beam CT Scan
Even if the dentist tells you that your case is simple, you are well advised to obtain a second opinion with a Cone Beam CT scan (CBCT), before the procedure. Many dentists and oral surgeons continue to argue that CT scans and CBCT scans are not the standard of care for diagnostic treatment planning before extractions and implant placement, even though periodontists have been using CT scans for years to avoid injuring the lingual and inferior alveolar nerves. Each dentist should inform their patient of the benefit of CT scans and Cone Beam CT Scans which provide more accurate information to the treating dentist who is performing an extraction of a posterior mandibular molar (lower jaw) or placing implants. The cost of a Cone Beam CT Scan is so reasonable now (about $350.00) and the risk of serious nerve injury or implant failure is significant enough to make this an easy decision for the patient. Unfortunately, either the hubris of the dentist or the lack of good information for the patient can result in avoidable nerve injuries occurring. CBCT has the benefit to patients of reducing radiation dose offered by this type of imaging over conventional CT scanning, improving the evaluation of the anatomical relationship of the inferior alveolar nerve/mandibular canal and the position of third molars. CBCT scans allow the dentist/oral surgeon to gain an appreciation in all dimensions of the precise relationship between the inferior alveolar canal and mandibular third molar. This enhanced understanding of anatomical relationships may result in the dentist referring the patient to an oral surgeon or aid the oral surgeon in determining the best surgical approach to the removal of the tooth reduce the risk of injuring the inferior alveolar nerve.
Every well informed patient will understand the benefits of a Cone Beam CT Scan (CBCT), and will insist on a CBCT before their dentist performs the extraction or implant placement . I have already compared the effective imaging of a panorex x-ray, periapical x-ray and a CBCT x-ray when used by a dentist to gage the appropriate length of an implant to replace a missing tooth in the second molar position (see Negligent Implant Placement). It is important to understand that a panorex and periapical x-ray only provide two-dimensional information to the dentist. The dentist can approximate the length of the implant with these x-rays, but the periapical x-ray is limited in the area that is viewed and the panorex provides a distorted radiograph when it reduces a three dimensional object (the upper and lower jaw) into a two dimensional radiograph. Think of the distortion of reducing a globe of the earth into a two dimensional map. The thickness of the bone and the location of the mandibular canal cannot be accurately determined in space without a three dimensional x-ray, either CT Scan or CBCT. Let us compare these three dimensional radiographs.
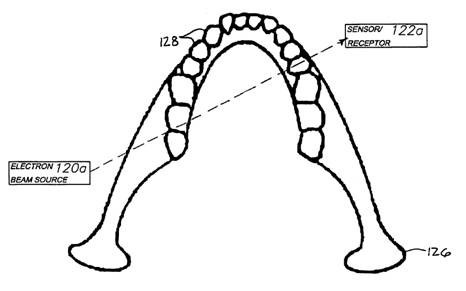
The CT Scan device (Image #21) uses a narrow fan beam (Image #22) that rotates around the object acquiring one or more thin slices with each rotation. The CT Scan makes multiple rotations around the patient and obtains a good contrast resolution.
Image #1: CT Scanner

Image #2: CT Scanner fan beam method of radiographic capture

Image #3 CT slice
The Cone-beam scanning device (Image #24) uses a cone-shaped beam to capture super high resolution radiographic imaging in a single rotation around the patient (Image #25) with less radiation exposure (1/7 of a regular Ct Scan and 1.6x a panorex) (Image #26) and greater detail(spatial resolution down to 0.80 mm).
Image #4 Accuitomo Cone Beam CT Scanner
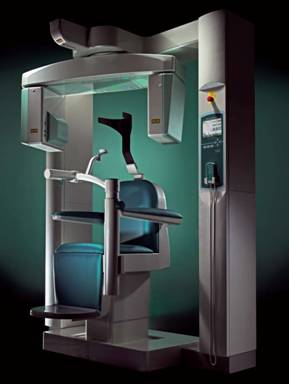
Image #5 Cone Beam Imaging

Image #6 Radiation Dosage Comparison (the NewTom and the I-CAT are both CBCT devices)

The important difference between a CT scan and a CBCT is the resolution at a fraction of the radiation dose. It is safer and provides the best resolution that you can have. Compare the resolution of the below CT scan showing an implant in the mandibular canal with software (Image #27), with the CBCT image and the reconstruction of the skull with detailed images below.
Image #7: Simplant rendition of CT scan of implant in mandibular canal
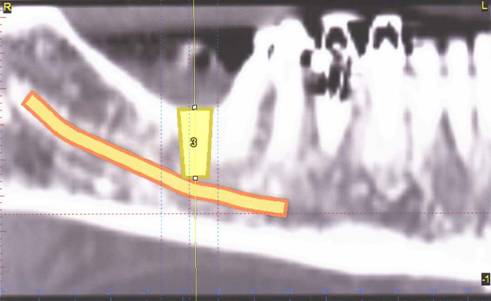
Image #8: Simplant rendition of CBCT scan of implants in mandibular canal
Panorex x-rays and periapical x-rays are used as screening radiographs preoperatively to evaluate patient’s for implant depth and to rule out the close proximity of the third molar roots to the inferior alveolar nerve. However, when these radiographs demonstrate an increase risk of injury to the inferior alveolar nerve, a CBCT should be ordered. In 2010, a study compared panorex x-rays which demonstrated an increased risk of inferior alveolar injury from third molar extraction with CBCT scans of the same third molars. The following panoramic radiographic findings were found to be indicative of significantly increased risk of inferior alveolar nerve injury.
- Darkening of the root
- Interruption of the radiopaque line
- Diversion of the inferior alveolar canal
Radiographic studies from panoramic x-rays and CBCT scans for these high risk extractions were compared and demonstrated the value of the CBCT in reducing injury to the inferior alveolar nerve when in close proximity to the third molars roots. The following are some of these examples:
Image #9: Panoramic radiograph with darkening across the lower left root of the third molar with schematic diagram (canal in green).

Image #9a: CBCT image of the third molar seen in Image #29 above. Note the buccal/cheek position of the nerve (dark yellow) with no contact with the root.
Image #10: Panoramic image of lower right third molar exhibiting darkening of the root as the inferior alveolar nerve overlaps.

Image #11: Coronal CBCT of panoramic x-ray in Image #31 Note buccal/cheek position of the inferior alveolar nerve and the thinned lingual plate which creates its own risk of fracture and injury to the lingual nerve on the other side of the lingual plate.
The advantage of the CBCT scan when compared with the panoramic view of the same third molar is that once the inferior alveolar nerve is located in three dimensional space and the surrounding landmarks are assessed, the oral surgeon is in a better position to devise an appropriate surgical approach to the surgical extraction of the patient’s third molar.

